Understanding Your Procedure
Lung Volume Reduction
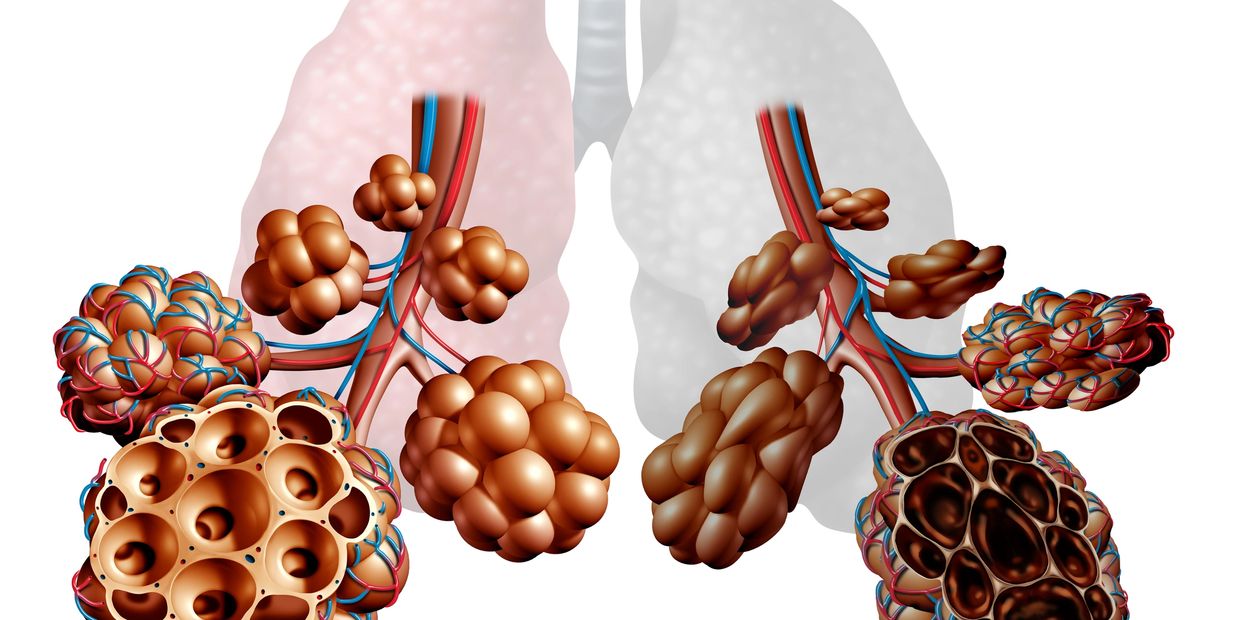
Imagine your lungs as balloons. In conditions like emphysema, these balloons are over-inflated, making it hard for you to breathe. In Lung Volume Reduction (LVR), parts of these over-inflated “balloons” are excluded or surgically removed, making more room in the chest for the healthier parts of the lungs to expand. This can make breathing easier. It’s like going from trying to breathe through a straw to breathing normally. This can significantly improve your quality of life. Here we’ll explore the different types of lung volume reduction techniques, risks, benefits, expected recovery, and possible post-operative complications.
Discuss your concerns
Advice, support, and guidance on condition management, understanding diagnoses and treatment options, lifestyle adjustments, and accessing financial aid.
Types of Lung Volume Reduction Procedures

Lung Volume Reduction Surgery (LVRS)
Lung Volume Reduction Surgery (LVRS) is a surgical procedure designed to improve breathing in patients with severe emphysema, a type of Chronic Obstructive Pulmonary Disease (COPD). The procedure involves the removal of the most damaged parts of the lungs, allowing the healthier parts to expand and function more effectively. The surgery is performed under general anesthesia. The surgeon makes incisions on either side of the chest to access the lungs and removes up to 30% of the most diseased lung tissue. The remaining lung tissue can then expand more fully, and the diaphragm and other muscles used in breathing return to a more normal position, making breathing easier. LVRS can significantly improve quality of life for patients with severe emphysema. Benefits include improved lung function, reduced breathlessness, increased ability to exercise, and enhanced overall quality of life. Some studies have also shown that LVRS can increase life expectancy for certain groups of patients. However, LVRS is a major operation and, like all surgeries, it has risks, including complications from anaesthesia, infection, and a prolonged recovery period. Therefore, it’s typically reserved for those who have severe symptoms but do not respond to medical therapy. It’s important to note that LVRS is not a cure for emphysema, but it can help manage the symptoms and improve the patient’s quality of life. Patients will still need to use medications and oxygen as prescribed by their doctor, and it’s crucial that they stop smoking before the surgery and do not start again afterwards.
Bronchoscopic Lung Volume Reduction (BLVR)
Bronchoscopic Lung Volume Reduction (BLVR) is a minimally invasive procedure developed in the early 2000s as a treatment for severe Chronic Obstructive Pulmonary Disease (COPD), primarily caused by emphysema. BLVR involves the use of endobronchial valves, coils, or thermal vapour ablation. Endobronchial valves are medical devices inserted using a bronchoscope into sections of the lungs damaged by emphysema. These valves allow air to exit these sections but not to re-enter, causing the damaged lung tissue to deflate and reducing the excessive lung volume (hyperinflation) caused by emphysema. Clinical research has found that BLVR confers measurable benefits, including improved lung function, improved exercise tolerance, and a lower risk of injury and infection. However, it also carries risks such as COPD exacerbation, respiratory failure, pneumothorax, and pneumonia.
Experimental Treatments
- Steam Ablation: This technique involves the use of steam to cause scarring and shrinkage in the less functional areas of the lung. A bronchoscope is used to deliver steam to targeted areas of the lung. The heat from the steam causes the affected lung tissue to scar and shrink, reducing the volume of the diseased lung. This allows the healthier parts of the lung to expand and function more effectively. The procedure is minimally invasive and can be performed under local anaesthesia, reducing the risk of complications and recovery time.
- Targeted Lung Denervation (TLD): TLD is a novel approach that involves disrupting the nerve supply to the smooth muscles in the airways. This can help to reduce airway constriction and improve lung function. The procedure is performed using a bronchoscope, which is inserted through the mouth or nose and into the lungs. A special catheter is then used to deliver radiofrequency energy to specific nerves in the lungs, disrupting their function. This can help to relax the airways and improve breathing.
- Lung Volume Reduction Coils (LVRC): LVRC is a minimally invasive procedure that involves the placement of nitinol coils into the airways of the diseased parts of the lung. The coils help to compress the diseased lung tissue and allow the healthier parts of the lung to expand and function more effectively. The procedure can lead to improvements in lung function, exercise capacity, and quality of life, although the results can vary greatly between patients.
- AeriSeal: The AeriSeal System is designed to limit collateral ventilation, which is caused by openings in the lung fissures, or walls between the lung lobes. The system works by occluding these naturally occurring openings in a lobe targeted for bronchoscopic lung volume reduction (BLVR), blocking collateral ventilation. Successful treatment with the AeriSeal System is followed by treatment with commercially available Zephyr Valves.
Operative Techniques
Robotic-Assisted Thoracoscopic Surgery (RATS)
Robotic-Assisted Thoracoscopic Surgery utilizes robotic arms that are under the surgeon’s control. This technique amplifies precision and agility during minimally invasive procedures. The use of CO2 inflation helps to expand the working area within the thoracic cavity, enhancing the visibility and maneuverability of the robotic instruments. This is especially advantageous in lung volume reduction surgery, where the surgical field is constrained due to hyperinflated lungs. The robot-assisted method also integrates the use of the Indocyanine Green (ICG) tracer for real-time Firefly Perfusion Assessment during surgery. When the ICG tracer is injected into the bloodstream, it can be visualized using near-infrared imaging, offering real-time imaging of vascular structures and tissue perfusion. This aids in pinpointing the lung areas with poor perfusion, which are typically the focus in lung volume reduction surgery.

Video-Assisted Thoracoscopic Surgery (VATS)
Video-Assisted Thoracoscopic Surgery provides numerous benefits over conventional open surgery. VATS is a less invasive surgical method that employs a small video camera, known as a thoracoscope, which is inserted through tiny incisions in the chest wall. This technique enables surgeons to view and operate on lung structures without the necessity for a large thoracotomy incision. VATS minimizes patient trauma, resulting in less pain after surgery, shorter hospital stays, faster recovery periods, and a lower risk of complications. In the realm of lung volume reduction surgery, VATS facilitates accurate identification and removal of the most diseased lung sections, enhancing lung function and patient quality of life. The application of reinforced staplers ensures a secure seal of lung tissue, thereby decreasing the risk of air leaks and the requirement for extended chest tube drainage.

Bronchoscopic Lung Volume Reduction (BLVR)
In Bronchoscopic Lung Volume Reduction, endobronchial valves are introduced into the lungs via a catheter inserted through a bronchoscope. The procedure entails the implantation of one-way valves into the airways that lead to the affected lung sections. These valves permit air to exit these sections but block its re-entry, resulting in the deflation of these areas and a decrease in hyperinflation. The procedure, which typically lasts an hour, involves administering anaesthesia intravenously. Post-procedure, patients generally stay in the hospital for a minimum of 48 hours. BLVR offers several benefits over traditional Lung Volume Reduction Surgery. It’s less invasive, thereby reducing the risk of complications and recovery time. It also eliminates the need for surgical cuts, reducing pain and discomfort. Furthermore, BLVR can be performed on patients who might not be eligible for LVRS due to various health considerations.

Common Risks
Bleeding
Infection
Infection
Risk of bleeding during or after surgery.
Infection
Infection
Infection
Post-surgery infections in the chest area.
Pain
Infection
Air Leak
Discomfort and soreness are common after the procedure.
Air Leak
Damage to Lung
Air Leak
Air escaping from the lung tissue may need additional management.
Damage to Lung
Damage to Lung
Damage to Lung
Accidental injury to lung tissue during surgery.
Pneumonia
Damage to Lung
Damage to Lung
Inflammation of lung tissue post-surgery.
Nerve Damage
Wound Infection
Nerve Damage
Possible harm to nerves near the surgical site.
Scarring
Wound Infection
Nerve Damage
Formation of scar tissue in the chest.
Wound Infection
Wound Infection
Scar Tissue Adhesions
Risk of infection at the surgical incision site.
Scar Tissue Adhesions
Scar Tissue Adhesions
Scar Tissue Adhesions
Formation of adhesions between lung and chest wall.
Mucus plugging
Scar Tissue Adhesions
Breathing Problems
Mucus that would typically clear from your lungs might accumulate in your airways.
Breathing Problems
Scar Tissue Adhesions
Breathing Problems
Difficulty breathing due to lung changes.
Valve related Complications
Pneumothorax
Granulation tissue formation
Granulation tissue formation
Pneumothorax is a common risk after valve placement; but doesn't negatively impact clinical outcomes. It can be managed with drain insertion.
Granulation tissue formation
Granulation tissue formation
Granulation tissue formation
Granulation tissue formation after endobronchial valve placement can lead to valve dysfunction and compromise the effectiveness of the treatment.
Improper valve placement
Granulation tissue formation
Improper valve placement
Improper valve placement may not effectively reduce lung volume and can result in ineffective treatment and complications related to airway obstruction.
Valve migration
Valve expectoration
Improper valve placement
Valve migration can lead to ineffective treatment as the valve may not block the intended airway. An additional procedure to reposition or remove the migrated valve will be required.
Valve expectoration
Valve expectoration
Valve expectoration
Valve expectoration can lead to ineffective treatment and will require an additional procedure for valve replacement. It’s important to seek medical attention if expectoration occurs.
Haemoptysis
Valve expectoration
Valve expectoration
Haemoptysis, or coughing up blood, can occur due to airway injury during the procedure, or airway irritation following the procedure. It's also possible that valves could exacerbate existing conditions in the lung.
COPD exacerbation
COPD exacerbation
COPD exacerbation
Chronic Obstructive Pulmonary Disease exacerbation could lead to worsening of respiratory symptoms, increased need for medication, hospitalization, and impact the overall effectiveness of volume reduction.
Pneumonia
COPD exacerbation
COPD exacerbation
Pneumonia can occur due to post-procedure infection or lung tissue injury. Severe cases may lead to respiratory failure, necessitating the need for intubation and mechanical ventilation, in an intensive care unit.
Rare Complications
Allergic reaction to anaesthesia
Allergic reaction to anaesthesia
Allergic reaction to anaesthesia
General anaesthesia-related complications.
Haemothorax
Allergic reaction to anaesthesia
Allergic reaction to anaesthesia
Accumulation of blood in the chest cavity.
Persistent Pain
Allergic reaction to anaesthesia
Surgical emphysema
Long-lasting discomfort after surgery.
Surgical emphysema
Surgical emphysema
Surgical emphysema
Air trapped under the skin, causing swelling and discomfort.
Empyema
Surgical emphysema
Blood Clots
An infection of the chest cavity, which can lead to serious pulmonary issues.
Blood Clots
Surgical emphysema
Blood Clots
Formation of blood clots in legs or lungs.
Bronchopleural Fistula
Bronchopleural Fistula
Bronchopleural Fistula
Abnormal connection between airways and pleura.
Atrial Fibrillation
Bronchopleural Fistula
Bronchopleural Fistula
An irregular heartbeat that typically develops between days two to four after surgery and is often temporary.
Respiratory Failure
Bronchopleural Fistula
Respiratory Failure
Severe lung dysfunction after surgery.
Heart Attack
Heart Attack
Respiratory Failure
Surgery can trigger cardiac events, including heart attacks, heart failure, and rhythm disturbances.
Stroke
Heart Attack
Stroke
Occurs during or after surgery, potentially leading to longer hospital stays and increased mortality or disability risk.
Death
Heart Attack
Stroke
Despite advantages, surgery carries mortality risk. Nearly three-quarters of post-surgery deaths occur without critical care admission.
Dr Periklis Perikleous, Consultant in Thoracic Surgery at St George's University Hospitals NHS Foundation Trust in London, United Kingdom
With practicing privileges at Spire St Anthony's Hospital in London, United Kingdom
Copyright © 2024 drperiklisperikleous.co.uk